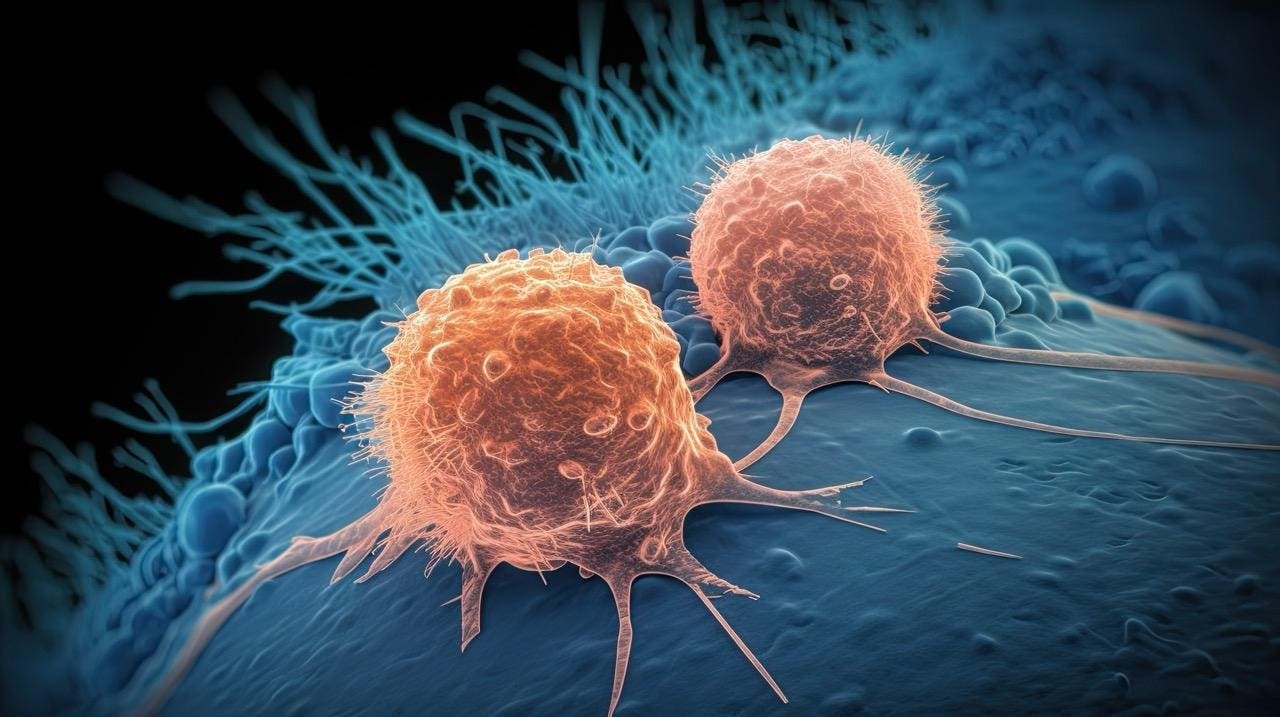
Cell-based cancer therapies, particularly CAR T-cell therapy, have shown remarkable success, but significant hurdles—high costs, lengthy treatment timelines, and reliance on individual patient cells—have limited their widespread adoption. New research demonstrates that these barriers may soon be overcome with the development of “off-the-shelf” universal donor cells.
The Promise of Universal Donor Cells
Traditional CAR T-cell therapy involves extracting a patient’s own immune cells, genetically modifying them to target cancer, and then reinfusing them. This process is slow, expensive (often exceeding several hundred thousand dollars per patient), and not always feasible for those with compromised immune systems. The solution lies in allogeneic cell therapies—modified immune cells from healthy donors that can be used for multiple patients. This approach promises faster, cheaper, and more accessible treatment.
How Universal Cells Work
The key to universal cell therapy is modifying donor T cells to prevent rejection by the recipient’s immune system. Researchers achieve this through gene editing, disabling the donor cells’ ability to attack each other and minimizing recognition by the patient’s body. These edited cells are then expanded, frozen, and stored in cell banks, ready for immediate use. This eliminates the need for patient-specific manufacturing, significantly reducing wait times and costs.
Recent Trial Results: Rapid Remission and Scalability
A study published in The New England Journal of Medicine evaluated this approach in 11 patients. All patients achieved remission within 28 days, with 9 reaching deep remission, enabling them to proceed to stem-cell transplants. This demonstrates the therapy’s potential for rapid and scalable delivery.
Challenges and Next Steps
While promising, universal cell therapy is not without risks. Patients experienced expected toxicities, including cytokine release syndrome, fever, and infections. Two patients with residual disease ultimately received palliative care, and some relapsed despite initial success. These findings underscore that this remains an intensive, high-risk approach.
Researchers are now focused on improving the durability of the therapy, reducing the need for immunosuppressant drugs, and investigating whether universal cells can cure patients without the need for subsequent transplantation. The transition from individualized to universal cell therapies is well underway.
Universal cell therapy represents a practical advance toward broader access to life-saving cancer treatments. Ongoing research is crucial to refine safety and long-term efficacy, but the potential for faster, cheaper, and more accessible care is now within reach.